Covid-19 Antibodies
Antibodies For SARS-CoV-2 Research
Antibodies are a critical part of COVID-19 research as they are used to gain insight into the immune system’s response to SARS-CoV-2 infections. The relevant applications of the antibodies include the detection of biomarkers such as cytokines or the detection of CD4 and CD8 T cells, as well as the inclusion in serological tests for the control of immunoglobulins. Our wide selection of trusted antibodies and related products includes reagents that may be relevant to support SARS-CoV-2 research. For research use only. It should not be used in diagnostic procedures.
Antibodies For The Detection Of Cytokine, CD4 And CD8
When the immune system detects a pathogen, such as SARS-CoV-2, it releases certain soluble substances in response. Viral infection can lead to an uncontrolled increase in cytokine levels known as a “cytokine storm.” The increase in the levels of biomarkers such as IL-10, IL-1β, IP-10, IFNγ and IL-1RA is considered an indication of the severity of the viral infection and has been shown in early studies to be associated with infection by SARS-CoV-2.
Another study found that IL-6 levels increased with SARS-CoV-2 infection. Other indicators of viral infection include increases in IFNα, IL-2RA, and C-reactive protein (CRP). An additional finding that is sometimes associated with SARS-CoV-2 infection is decreased levels of CD4 and CD8 T cells. Antibodies may be useful in studying the severity of the infection by detecting the level of cytokines, CD4 T cells and CD8 T cells.
Antibodies For Serological Monitoring
Antibody-based serology tests are useful in identifying subjects with an adaptive immune response to the SARS-CoV-2 virus. As with most infections, the antibody response to SARS-CoV-2 infection begins with the early production of IgM and/or IgA antibodies, followed by a more specific and longer-lasting IgG response.
Our portfolio offers a variety of antibodies for the detection of human immunoglobulin (Ig) for seroprevalence studies. It includes conjugated antibodies linked to a label and used for a wide range of assay techniques, such as detection, purification, classification and microscopy applications. Our antibodies are validated in various immune applications and a variety of hosts.
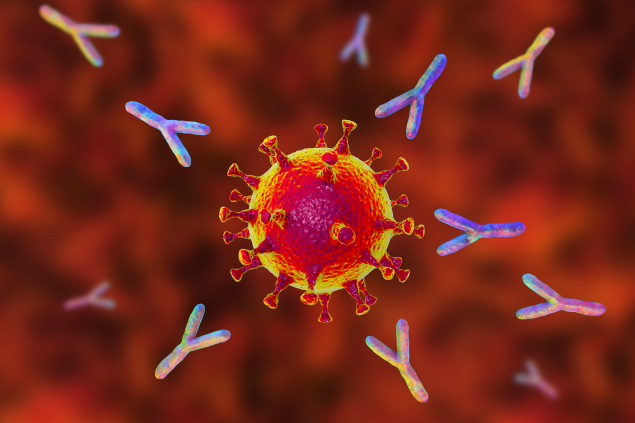
Antibodies and the immune system.
The immune system is a complex network of cells, tissues, and organs that work together to protect the body from infection.
Antibodies are proteins that your immune system makes to help fight infection and protect you from future disease.
When you are infected with a virus or bacteria, your immune system produces antibodies specifically to fight it. Your immune system can also learn to safely produce antibodies through vaccination. Once you have antibodies against a particular disease, they provide some protection against that disease. Even if you get sick, having antibodies can protect you from serious illness because your body has some experience fighting that illness. The duration of this protection may be different for each disease, each person or influenced by other factors. Antibodies are just one part of your immune response.
Antibodies and COVID-19
Antibodies to SARS-CoV-2, the virus that causes COVID-19, can be detected in the blood of people who have recovered from COVID-19 or people who have been vaccinated against COVID-19. Getting a vaccine is safer than getting COVID-19, and vaccination against COVID-19 antibodies is recommended for everyone over 5 years of age. If someone has already had COVID-19, vaccination against COVID-19 increases their body’s antibody response, which improves their protection.
It is important to remember that some people with SARS-CoV-2 antibodies may become infected after vaccination (vaccinal breakthrough infection) or after recovery from a previous infection (reinfected). Based on what we know at this time, the risk of reinfection is low for at least the first 6 months after a laboratory-diagnosed infection with the virus that causes COVID-19. When someone who is fully vaccinated gets COVID-19, it is called a vaccine advance infection. No vaccine is 100% effective, so some advanced infections are expected. The risk of infection, serious illness, hospitalization, and death is much lower for vaccinated people compared to unvaccinated people.
For many illnesses, including COVID-19, antibodies are expected to decline or “dwindle” over time. After a long enough period of time, your antibody level may drop below a level that provides effective protection. This level is called the “protection threshold”. When antibodies drop below the protective threshold, you can become more vulnerable to serious illness. We do not yet know what the protective threshold of antibodies to the virus that causes COVID-19 is or how long it takes for these antibodies to decline. Even after the antibodies subside, your immune system may have cells that remember the virus and can act quickly to protect you from serious illness if you become infected. These topics are being investigated by scientists around the world.
I have COVID-19 antibodies. What does that mean?
A positive antibody test result can help identify someone who has had COVID-19 in the past or has been vaccinated against COVID-19. Antibody tests are not used if you have symptoms of COVID-19 or to diagnose a current case of COVID-19. This is because it takes 1 to 3 weeks after contracting COVID-19 for most people with a healthy immune system to develop antibodies. A viral test is recommended to identify current infection with the virus that causes COVID-19. More information is available about the role and uses of antibody tests.
Most people who have a positive antibody test can continue with their normal activities, including work, but should still take steps to protect themselves and others, including vaccination. A positive antibody test result by itself, especially one from an infection at an unknown time or that was determined by a viral test more than 6 months ago, does not necessarily mean that you are immune from contracting COVID-19. If you have had an antibody test, it is important to review the test results with your health care provider.
How do scientists study antibodies?
The science of antibodies is called “serology.” Antibody tests also called “serology tests,” identify antibodies in blood samples. Although other parts of the immune system also contribute to the protection, it is easier to test for antibodies.
As of August 2021, more than 80 antibody tests external icons have received emergency use authorization (EUA) from the FDA to detect antibodies against SARS-CoV-2. Scientists are using these antibody tests to learn more about the level of antibodies needed to protect people from COVID-19 (threshold protection) and how long this protection lasts. The FDA does not currently recommend antibody tests for widespread and routine use in individual medical decision making while this information is being collected and evaluated. If you have questions about whether an antibody test is right for you, talk to your health care provider or your state or local health department.
Not all antibody tests identify the same antibodies. Some antibody tests are more or less sensitive to specific sections of the antibody protein than others. This means that different antibody tests may not have the same results, even when they are both testing for SARS-CoV-2 antibodies. Scientists use these differences in evidence to help answer different research questions about how the immune system responds to the virus that causes COVID-19 and to improve our understanding of COVID-19.
What information do SARS-CoV-2 antibodies give us about how to respond to COVID-19?
As scientists learn more about SARS-CoV-2 antibodies, we will understand much more about how to treat and control COVID-19. Serologic surveillance (studies that investigate antibodies in the population) provides information on how long antibody protection against COVID-19 lasts and whether this protection is different among people who have antibodies to the infection, compared to people who have antibodies from vaccination, or both.
We can also learn more about which groups of people might not make as many antibodies or keep them for as long as others, for example, people who are immunocompromised compared to people who have healthy immune systems. This is important information for making decisions about whether or not additional doses of vaccines or boosters are needed when they would be recommended, and who would need them first.